Heart Failure
- Heart failure (HF) is a frequent, potentially deadly and costly ($39 billion annually in the US2) condition, that often occurs as the end stage of cardiac disease.
- It affects 23 million people worldwide and is on the rise.2
- It is the leading cause of hospitalization for patients older than 65 years in the developed world.2
- One in 5 people die within one year of HF diagnosis and up to 50% die within 5 years.2
Definition
Heart failure (HF) is a complex clinical syndrome in which the heart’s pumping function becomes insufficient (ventricular dysfunction) to meet the oxygen demand of vital organs and tissues of the body. As a result, fluid builds up in the lung and/or various parts of the body causing congestion and edema. This explains common symptoms such as difficulty breathing, fatigue and poor exercise tolerance.
Heart Failure signs & symptoms chart
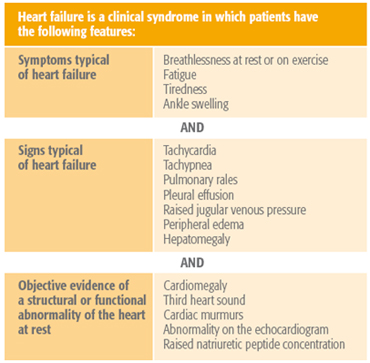
Adapted from: Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2008; 29: 2388-442
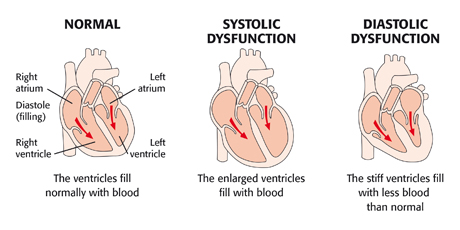
HF is a chronic disease that worsens over time, causing progressive remodeling of the heart. It changes the size and shape of the heart, impairing ventricular function in two ways:
- Systolic HF (HF with reduced ejection fraction): thinning and weakening of the ventricle walls results in dilation and a reduced capacity to eject blood.
- Diastolic HF (HF with preserved ejection fraction): thickening and stiffening of the ventricles due to hypertrophy results in impaired relaxation.
Diagnosis
Heart failure is diagnosed based on typical signs and symptoms as well as on objective evidence of structural or functional abnormality of the heart (ESC HF Guidelines 2012).
A rapid and accurate diagnosis is essential to target appropriate therapy and improve patient outcomes. However, HF is difficult to diagnose because the clinical symptoms are varied and often non-specific. The diagnosis must be based on a combination of patient history, physical examination, imaging and laboratory tests. Testing for biomarkers such as NT-proBNP and Galectin-3 helps early diagnosis and prognosis of heart failure3,4. Testing for Procalcitonin (PCT) is useful to diagnose concomitant bacterial pneumonia in patients presenting with acute HF.5
NT-proBNP - Early diagnosis of heart failure
NT-proBNP is the N-terminal fragment of B-type natriuretic peptide3. It is a proven biomarker for heart failure and is recommended in many guidelines as an integral part of the diagnostic work-up.6
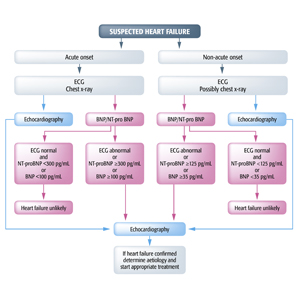
Diagnostic flowchart for patients with suspected heart failure-showing alternative 'echocardiography first' (blue) or 'natriuretic peptide first' (red) approaches
BNP = B-type natriuretic peptide; ECG = electrocardiogram; HF = heart failure; MR-proANP = mid-regional pro atrial natriuretic peptide; NT-proBNP = N-terminal pro B-type natriuretic peptide.
Source: McMurray JJ, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. Eur Heart J. 2012;33:1787-847
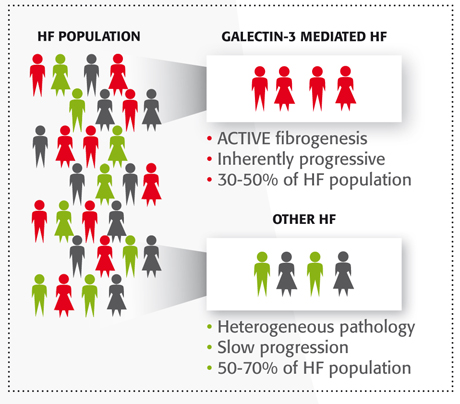
Galectin-3 – Identify high-risk patients
While NT-proBNP is a biomarker that helps diagnose heart failure, additional information is needed to phenotype HF patients at increased risk of re-hospitalization/mortality. It is now known that 30-50% of heart failure patients have an inherently progressive form of the disease mediated by high levels of Galectin-3.4 Galectin-3 causes progressive fibrosis, known to be an underlying pathology in heart failure7. Measuring Galectin-3 can provide information to optimize patient care decisions.4
Procalcitonin (PCT) - Diagnosis of concomitant bacterial pneumonia in HF patients
Concomitant cardiac and respiratory disorders occur in approximately 10% of patients with acute dyspnea8. Procalcitonin has recently been considered as a useful biomarker in the diagnosis of concomitant bacterial pneumonia in HF patients5.
Detecting superimposed pneumonia in patients presenting with AHF is difficult, since clinical signs are similar. The combined use of natriuretic peptides (BNP/NT-proBNP*) and PCT can help distinguish between pneumonia and AHF5.
Patients with HF are at increased risk for pneumonia9. It is important to identify acute heart failure (AHF) patients who are also superimposed with a bacterial infection (pneumonia), since they are at risk of worse outcome if not properly diagnosed and treated10.
* BNP was used in this study, but similar results are expected for the combination of PCT and NT-proBNP
Prevention/Treatment
Prevention
The best way to prevent heart failure is to maintain a healthy lifestyle that reduces well-known risk factors like high blood pressure and coronary artery disease.
Some of the things you can do to improve your chances of not developing heart failure include:
- Do not smoke
- Stay physically active
- Eat a well-balanced diet low in sugar, salt and saturated fats
- Maintain a healthy weight
- Reducing and managing stress
- If you have or are at risk for certain conditions, such as high blood pressure, high cholesterol and diabetes, work with your doctor to control these, including medication if necessary
Treatment
The recommended treatment for heart failure depends on the stage and severity. Therapeutic management controls risk factors and addresses the underlying causes/aggravating factors. It is aimed at providing symptom relief and preventing disease progression.
There are major evidence-based drug treatments for HF that target the various pathophysiological mechanisms that operate in HF and involve the heart, kidneys and peripheral circulation.
These drugs include:
- Diuretics to decrease the volume of fluid in the bloodstream
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) to promote vasodilatation
- Beta-blockers to slow the heart rate and block excessive stimulation of the heart
- Aldosterone receptor antagonists to lower blood pressure and reduce congestion
- Digoxin, inotropes may also be required in certain cases to stimulate heart contractions
“Measurement of biomarkers of myocardial fibrosis”, such as galectin-3, “may be considered for additive risk stratification in ambulatory and hospitalized HF patients”.
American College of Cardiology Foundation (ACCF) and the American Heart Association (AHA) 2013 Guideline for the Management of Heart Failure.
Depending on the degree of damage to the heart, surgery may be necessary (valve replacement, pacemaker, ventricular assistance device). In the case of severe damage, heart transplantation often remains the only cure.
Guidelines
- American College of Cardiology Foundation (ACCF) and the American Heart Association (AHA) 2013 Guideline for the Management of Heart Failure.
http://circ.ahajournals.org/content/early/2013/06/03/CIR.0b013e31829e8807 - European Society of Cardiology (ESC)
McMurray JJ, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787–1847 (link)
http://eurheartj.oxfordjournals.org/content/early/2012/05/17/eurheartj.ehs104Thygesen K, et al.; Study Group on Biomarkers in Cardiology of the ESC Working Group on Acute Cardiac Care. Recommendations for the use of natriuretic peptides in acute cardiac care: a position statement from the Study Group on Biomarkers in Cardiology of the ESC Working Group on Acute Cardiac Care. Eur Heart J. 2012;33:2001-6. (link)
http://eurheartj.oxfordjournals.org/content/early/2011/02/02/eurheartj.ehq509.full.pdf
- National Academy of Clinical Biochemistry (NACB)
Tang W.H. et al., National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: Clinical Utilization of Cardiac Biomarker Testing in Heart Failure. Circulation 2007; 116: 99-109 (link)
http://www.ncbi.nlm.nih.gov/pubmed/17630410Apple F.S. et al., National Academy of Clinical Biochemistry and IFCC committee for Standardization of Markers of Cardiac Damage Laboratory Medicine Practice Guidelines: Analytical Issues for Biomarkers of Heart Failure. Circulation 2007; 116: 95-98. (link)
http://circ.ahajournals.org/content/115/13/e352.full?ijkey=00965a64f6cd75a5736dc0161fd0ceddf87b268e&keytype2=tf_ipsecsha
- Heart Failure Society of America (HFSA)
Lindenfeld J, et al. HFSA 2010 Comprehensive Heart Failure Practice Guideline. J Card Fail. 2010;16:e1-194.
http://www.onlinejcf.com/article/S1071-9164(10)00173-9/abstract - American College of Emergency Physicians (ACEP)
Silvers SM, et al. Clinical Policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute heart failure syndromes. Ann Emerg Med 2007; 49: 627-669. (link)
http://www.annemergmed.com/article/S0196-0644(06)02461-9/fulltext
References
- Heidenreich PA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606-19.
- Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011;8:30-41.
- Thygesen K, et al.; Study Group on Biomarkers in Cardiology of the ESC Working Group on Acute Cardiac Care. Recommendations for the use of natriuretic peptides in acute cardiac care: a position statement from the Study Group on Biomarkers in Cardiology of the ESC Working Group on Acute Cardiac Care. Eur Heart J. 2012;33:2001-6.
- McCullough PA, Olobatoke A, Vanhecke TE. Galectin-3: a novel blood test for the evaluation and management of patients with heart failure. Rev Cardiovasc Med. 2011;12:200-10.
- Maisel A, et al. Use of procalcitonin for the diagnosis of pneumonia in patients presenting with a chief complaint of dyspnoea: results from the BACH (Biomarkers in Acute Heart Failure) trial. Eur J Heart Fail. 2012; 14: 278–286.
- McMurray JJ, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787-847
- de Boer RA, et al. Galectin-3: a novel mediator of heart failure development and progression. Eur J Heart Fail. 2009;11:811-7.
- Arenja N, et al. The ESC Textbook of Intensive and Acute Cardiac Care 2011: Acute Dyspnea
- Mor A, et al. Chronic heart failure and risk of hospitalization with pneumonia: a population-based study. Eur J Intern Med. 2013;24:349-53.
- Thomsen RW, et al. The impact of pre-existing heart failure on pneumonia prognosis: population-based cohort study. J Gen Intern Med. 2008;23:1407-13.
This Site is Not a Source of Medical Advice
The Healthcare Content of this Site is presented in summary form, is general in nature, and is provided for informational purposes only. It is not intended nor recommended to be used as a substitute for professional medical advice. You should not use the Healthcare Content of this Site for diagnosing a health or fitness problem or disease. Always seek the advice of your physician or other qualified health provider regarding any medical condition or treatment. Nothing contained on this Site is intended to be for medical diagnosis or treatment. It should not be used by physicians as a single source of information for making prescribing decisions. Never disregard medical advice or delay in seeking it because of something you have read on this Site.